Study Blue Which of the Following Results Isare Typical in Stage 3 Iron Deficiency Anemia
Iron deficiency is the most common cause of anemia and usually results from blood loss; malabsorption, such as with celiac disease, is a much less common cause. Symptoms are usually nonspecific. Red blood cells tend to be microcytic and hypochromic, and iron stores are low, as shown by low serum ferritin and low serum iron levels with high serum total iron-binding capacity. If the diagnosis is made, occult blood loss should be suspected until proven otherwise. Treatment involves iron replacement and treatment of the cause of blood loss.
Iron is distributed in active metabolic and storage pools. Total body iron is about 3.5 g in healthy men and 2.5 g in women; the difference relates to women's smaller body size and dearth of stored iron because of iron loss due to menses. The distribution of body iron is
-
Hemoglobin: 2 g (men), 1.5 g (women)
-
Ferritin: 1 g (men), 0.6 g (women)
-
Hemosiderin: 300 mg
-
Myoglobin: 200 mg
-
Tissue enzymes (heme and nonheme): 150 mg
-
Transport-iron compartment: 3 mg
Iron is absorbed in the duodenum and upper jejunum. Iron absorption is determined by its source and by what other substances are ingested with it. Iron absorption is best when food contains heme iron (meat). Dietary nonheme iron is usually in the ferric state (+3) and must be reduced to the ferrous state (+2) and released from food binders by gastric secretions. Nonheme iron absorption is reduced by other food items (eg, vegetable fiber phytates and polyphenols; tea tannates, including phosphoproteins; bran) and certain antibiotics (eg, tetracycline). Ascorbic acid is the only common food element known to increase nonheme iron absorption.
Iron from intestinal mucosal cells is transferred to transferrin, an iron-transport protein synthesized in the liver; transferrin can transport iron from cells (intestinal, macrophages) to specific receptors on erythroblasts, placental cells, and liver cells. For heme synthesis, transferrin transports iron to the erythroblast mitochondria, which insert the iron into protoporphyrin IX for it to become heme. Transferrin (plasma half-life, 8 days) is extruded for reutilization. Synthesis of transferrin increases with iron deficiency but decreases with any type of chronic disease.
Iron not used for erythropoiesis is transferred by transferrin to the storage pool; iron is stored in 2 forms:
-
Ferritin
-
Hemosiderin
The most important is ferritin (a heterogeneous group of proteins surrounding an iron core), which is a soluble and active storage fraction located in the liver (in hepatocytes), bone marrow, and spleen (in macrophages); in red blood cells (RBCs); and in serum. Iron stored in ferritin is readily available for any body requirement. Circulating (serum) ferritin level parallels the size of the body stores (1 ng/mL = 8 mg of iron in the storage pool).
The 2nd storage pool of iron is in hemosiderin, which is relatively insoluble and is stored primarily in the liver (in Kupffer cells) and in the bone marrow (in macrophages).
Because iron absorption is so limited, the body recycles and conserves iron. Transferrin binds and recycles available iron from aging RBCs undergoing phagocytosis by mononuclear phagocytes. This mechanism provides about 97% of the daily iron needed (about 2.5 mg of iron).
Severe and prolonged iron deficiency also may cause dysfunction of iron-containing cellular enzymes.
-
Nemeth E, Tuttle MS, Powelson J, et al: Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science 306(5704):2090–2093, 2004.
Because nonheme iron is poorly absorbed, dietary iron barely meets the daily requirement for most people. Even so, men who eat a typical Western diet are unlikely to become iron deficient solely as a result of dietary deficiency. However, even modest losses, increased requirements, iatrogenic phlebotomy, or decreased caloric intake can contribute to iron deficiency.
Blood loss is the major cause of iron deficiency. In men and postmenopausal women, the most frequent cause is chronic occult bleeding, usually from the gastrointestinal tract (eg, due to peptic ulcer disease Peptic Ulcer Disease A peptic ulcer is an erosion in a segment of the gastrointestinal mucosa, typically in the stomach (gastric ulcer) or the first few centimeters of the duodenum (duodenal ulcer), that penetrates... read more  , malignancy, hemorrhoids, or vascular ectasias Vascular Gastrointestinal Lesions Several distinct congenital or acquired syndromes involve abnormal mucosal or submucosal blood vessels in the gastrointestinal tract. These vessels may cause recurrent bleeding, which is rarely... read more
, malignancy, hemorrhoids, or vascular ectasias Vascular Gastrointestinal Lesions Several distinct congenital or acquired syndromes involve abnormal mucosal or submucosal blood vessels in the gastrointestinal tract. These vessels may cause recurrent bleeding, which is rarely... read more  ). In premenopausal women, cumulative menstrual blood loss (mean, 0.5 mg iron/day) is a common cause. Intestinal bleeding due to hookworm infection Symptoms and Signs Ancylostomiasis is infection with the hookworm Ancylostoma duodenale or Necator americanus. Symptoms include rash at the site of larval entry and sometimes abdominal pain or other... read more
). In premenopausal women, cumulative menstrual blood loss (mean, 0.5 mg iron/day) is a common cause. Intestinal bleeding due to hookworm infection Symptoms and Signs Ancylostomiasis is infection with the hookworm Ancylostoma duodenale or Necator americanus. Symptoms include rash at the site of larval entry and sometimes abdominal pain or other... read more  is a common cause in developing countries. Less common causes include urinary blood loss, recurrent pulmonary hemorrhage (see Diffuse Alveolar Hemorrhage Diffuse Alveolar Hemorrhage Diffuse alveolar hemorrhage is persistent or recurrent pulmonary hemorrhage. There are numerous causes, but autoimmune disorders are most common. Most patients present with dyspnea, cough, hemoptysis... read more
is a common cause in developing countries. Less common causes include urinary blood loss, recurrent pulmonary hemorrhage (see Diffuse Alveolar Hemorrhage Diffuse Alveolar Hemorrhage Diffuse alveolar hemorrhage is persistent or recurrent pulmonary hemorrhage. There are numerous causes, but autoimmune disorders are most common. Most patients present with dyspnea, cough, hemoptysis... read more  ) and chronic intravascular Myelodysplastic Syndrome (MDS) The myelodysplastic syndrome (MDS) is group of clonal hematopoietic stem cell disorders typified by peripheral cytopenia, dysplastic hematopoietic progenitors, a hypercellular or hypocellular... read more or traumatic (exercise-induced) hemolysis when the amount of iron released during hemolysis exceeds the plasma haptoglobin-binding capacity.
) and chronic intravascular Myelodysplastic Syndrome (MDS) The myelodysplastic syndrome (MDS) is group of clonal hematopoietic stem cell disorders typified by peripheral cytopenia, dysplastic hematopoietic progenitors, a hypercellular or hypocellular... read more or traumatic (exercise-induced) hemolysis when the amount of iron released during hemolysis exceeds the plasma haptoglobin-binding capacity.
Decreased iron absorption can result from gastrectomy or malabsorption syndromes Overview of Malabsorption Malabsorption is inadequate assimilation of dietary substances due to defects in digestion, absorption, or transport. Malabsorption can affect macronutrients (eg, proteins, carbohydrates, fats)... read more such as celiac disease Celiac Disease Celiac disease is an immunologically mediated disease in genetically susceptible people caused by intolerance to gluten, resulting in mucosal inflammation and villous atrophy, which causes malabsorption... read more  , atrophic gastritis Autoimmune Metaplastic Atrophic Gastritis Autoimmune metaplastic atrophic gastritis is an inherited autoimmune disease that attacks parietal cells, resulting in hypochlorhydria and decreased production of intrinsic factor. Consequences... read more
, atrophic gastritis Autoimmune Metaplastic Atrophic Gastritis Autoimmune metaplastic atrophic gastritis is an inherited autoimmune disease that attacks parietal cells, resulting in hypochlorhydria and decreased production of intrinsic factor. Consequences... read more  , Helicobacter pylori infection Helicobacter pylori Infection Helicobacter pylori is a common gastric pathogen that causes gastritis, peptic ulcer disease, gastric adenocarcinoma, and low-grade gastric lymphoma. Infection may be asymptomatic or... read more , achlorhydria, short bowel syndrome Short Bowel Syndrome Short bowel syndrome is malabsorption resulting from extensive resection of the small bowel (usually more than two thirds the length of the small intestine). Symptoms depend on the length and... read more , and rarely IRIDA Iron-transport deficiency anemia In myelodysplastic syndrome, anemia is commonly prominent. The anemia is usually normocytic or macrocytic, and a dimorphic (large and small) population of circulating cells can be present. ... read more (iron-refractory iron deficiency anemia). Rarely, absorption is decreased by dietary deprivation due to undernutrition.
, Helicobacter pylori infection Helicobacter pylori Infection Helicobacter pylori is a common gastric pathogen that causes gastritis, peptic ulcer disease, gastric adenocarcinoma, and low-grade gastric lymphoma. Infection may be asymptomatic or... read more , achlorhydria, short bowel syndrome Short Bowel Syndrome Short bowel syndrome is malabsorption resulting from extensive resection of the small bowel (usually more than two thirds the length of the small intestine). Symptoms depend on the length and... read more , and rarely IRIDA Iron-transport deficiency anemia In myelodysplastic syndrome, anemia is commonly prominent. The anemia is usually normocytic or macrocytic, and a dimorphic (large and small) population of circulating cells can be present. ... read more (iron-refractory iron deficiency anemia). Rarely, absorption is decreased by dietary deprivation due to undernutrition.
Symptoms and Signs of Iron Deficiency Anemia
In addition to the usual manifestations of anemia, some uncommon symptoms occur in severe iron deficiency. Patients may have pica Pica Pica is persistent eating of nonnutritive, nonfood material for ≥1 month when it is developmentally inappropriate (eg, pica is not diagnosed in children 2 years) and when it is not part of a... read more , an abnormal craving to eat nonfood substances (eg, ice, dirt, paint, starch, ashes). Other symptoms of severe deficiency include glossitis, cheilosis, and concave nails (koilonychia).
-
Complete blood count (CBC), serum iron, iron-binding capacity, serum ferritin, transferrin saturation, reticulocyte count, red cell distribution width (RDW), and a peripheral blood smear
-
Rarely bone marrow examination
Iron deficiency anemia is suspected in patients with chronic blood loss or microcytic anemia, particularly if pica is present. In such patients, a CBC, serum iron and iron-binding capacity, and serum ferritin and reticulocyte count are obtained (see table Typical Serum Values for Iron, Iron-Binding Capacity, Ferritin, and Transferrin Saturation Typical Normal Serum Values for Iron, Iron-Binding Capacity,Ferritin, and Transferrin Saturation ![]() ).
).
Serum ferritin levels closely correlate with total body iron stores. The range of normal in most laboratories is 30 to 300 ng/mL (67.4 to 674.1 pmol/L), and the mean is 88 ng/mL (197.7 pmol/L) in men and 49 ng/mL (110.1 pmol/L) in women. Low levels (< 12 ng/mL [27 pmol/L]) are specific for iron deficiency. However, ferritin is an acute-phase reactant, and levels increase in inflammatory and infectious disorders (eg, hepatitis Overview of Acute Viral Hepatitis Acute viral hepatitis is diffuse liver inflammation caused by specific hepatotropic viruses that have diverse modes of transmission and epidemiologies. A nonspecific viral prodrome is followed... read more ), and neoplastic disorders (especially acute leukemia Overview of Leukemia Leukemia is a malignant condition involving the excess production of immature or abnormal leukocytes, which eventually suppresses the production of normal blood cells and results in symptoms... read more , Hodgkin lymphoma Hodgkin Lymphoma Hodgkin lymphoma is a localized or disseminated malignant proliferation of cells of the lymphoreticular system, primarily involving lymph node tissue, spleen, liver, and bone marrow. Symptoms... read more  , and gastrointestinal tract tumors). In these disorders, a serum ferritin level up to 100 ng/mL remains compatible with iron deficiency.
, and gastrointestinal tract tumors). In these disorders, a serum ferritin level up to 100 ng/mL remains compatible with iron deficiency.
The reticulocyte count is low in iron deficiency. The peripheral smear generally reveals hypochromic red cells with significant anisopoikilocytosis, which is reflected in a high red cell distribution width (RDW).
The most sensitive and specific criterion for iron-deficient erythropoiesis is absent bone marrow stores of iron, although a bone marrow examination is rarely needed.
Laboratory test results help stage iron deficiency anemia.
Stage 1 is characterized by decreased bone marrow iron stores; hemoglobin (Hb) and serum iron remain normal, but the serum ferritin level falls to < 20 ng/mL (44.9 pmol/L). The compensatory increase in iron absorption causes an increase in iron-binding capacity (transferrin level).
During stage 2, erythropoiesis is impaired. Although the transferrin level is increased, the serum iron level decreases; transferrin saturation decreases. Erythropoiesis is impaired when serum iron falls to < 50 mcg/dL (< 9 micromol/L) and transferrin saturation to < 16%. The serum transferrin receptor level rises (> 8.5 mg/L).
During stage 3, anemia with normal-appearing RBCs and indices develops.
During stage 4, microcytosis and then hypochromia develop.
During stage 5, iron deficiency affects tissues, resulting in symptoms and signs.
Diagnosis of iron deficiency anemia prompts consideration of its cause, usually bleeding. Patients with obvious blood loss (eg, women with menorrhagia) may require no further testing. Men and postmenopausal women without obvious blood loss should undergo evaluation of the gastrointestinal (GI) tract, because anemia may be the only indication of an occult GI cancer. Rarely, chronic epistaxis or genitourinary bleeding is underestimated by the patient and requires evaluation in patients with normal GI study results.
Iron deficiency anemia must be differentiated from other microcytic anemias (see table Differential Diagnosis of Microcytic Anemia Due to Decreased RBC Production Differential Diagnosis of Microcytic Anemia Due to Decreased Red Blood Cell Production ![]() ). If tests exclude iron deficiency in patients with microcytic anemia, then the anemia of chronic disease Anemia of Chronic Disease The anemia of chronic disease is a multifactorial anemia. Diagnosis generally requires the presence of a chronic inflammatory condition, such as infection, autoimmune disease, kidney disease... read more and structural Hb abnormalities (eg, hemoglobinopathies Sickle Cell Disease Sickle cell disease (a hemoglobinopathy) causes a chronic hemolytic anemia occurring almost exclusively in people with African ancestry. It is caused by homozygous inheritance of genes for hemoglobin... read more
). If tests exclude iron deficiency in patients with microcytic anemia, then the anemia of chronic disease Anemia of Chronic Disease The anemia of chronic disease is a multifactorial anemia. Diagnosis generally requires the presence of a chronic inflammatory condition, such as infection, autoimmune disease, kidney disease... read more and structural Hb abnormalities (eg, hemoglobinopathies Sickle Cell Disease Sickle cell disease (a hemoglobinopathy) causes a chronic hemolytic anemia occurring almost exclusively in people with African ancestry. It is caused by homozygous inheritance of genes for hemoglobin... read more 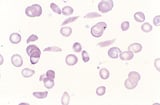 ) are considered. Clinical features, Hb studies (eg, Hb electrophoresis and Hb A2), and genetic testing (eg, for alpha-thalassemia Alpha-thalassemia Thalassemias are a group of inherited microcytic, hemolytic anemias characterized by defective hemoglobin synthesis. Alpha-thalassemia is particularly common among people with African, Mediterranean... read more ) may help distinguish these entities.
) are considered. Clinical features, Hb studies (eg, Hb electrophoresis and Hb A2), and genetic testing (eg, for alpha-thalassemia Alpha-thalassemia Thalassemias are a group of inherited microcytic, hemolytic anemias characterized by defective hemoglobin synthesis. Alpha-thalassemia is particularly common among people with African, Mediterranean... read more ) may help distinguish these entities.
-
Oral supplemental iron
-
Rarely parenteral iron
Iron therapy without pursuit of the cause is poor practice; a bleeding site should be sought even in cases of mild anemia.
Oral or parenteral iron therapy should continue for ≥ 6 months after correction of hemoglobin levels to replenish tissue stores.
The response to treatment is assessed by serial Hb measurements until normal RBC values are achieved. Hb rises little for 2 weeks but then rises 0.7 to 1 g/week until near normal, at which time the rate of increase tapers. Anemia should be corrected within 2 months. A subnormal response suggests continued hemorrhage, underlying infection or cancer, insufficient iron intake, or malabsorption of oral iron. If the symptoms of anemia, such as fatigue, weakness, and shortness of breath, do not abate following resolution of the anemia, an alternative cause should be sought.
-
1. Moretti D, Goede JS, Zeder C, et al: Oral iron supplements increase hepcidin and decrease iron absorption from daily or twice-daily doses in iron-depleted young women. Blood 126(17):1981-1989, 2015. doi: 10.1182/blood-2015-05-642223
-
Iron deficiency anemia is usually caused by blood loss (eg, gastrointestinal, menstrual) but may be due to hemolysis, malabsorption, or increased demand for iron (eg, in pregnancy, lactation, periods of rapid growth in children).
-
Differentiate iron deficiency anemia from other microcytic anemias (eg, anemia of chronic disease, hemoglobinopathies).
-
Measure serum iron, iron-binding capacity, and serum ferritin levels.
-
Iron deficiency typically causes low serum iron, high iron-binding capacity, and low serum ferritin levels.
-
Always seek a cause of iron deficiency, even when anemia is mild.
-
Oral iron supplements are usually adequate; reserve use of parenteral iron for hematologists because of risks of adverse effects (eg, infusion reactions and rare anaphylactoid reactions).
Source: https://www.msdmanuals.com/professional/hematology-and-oncology/anemias-caused-by-deficient-erythropoiesis/iron-deficiency-anemia